Introduction
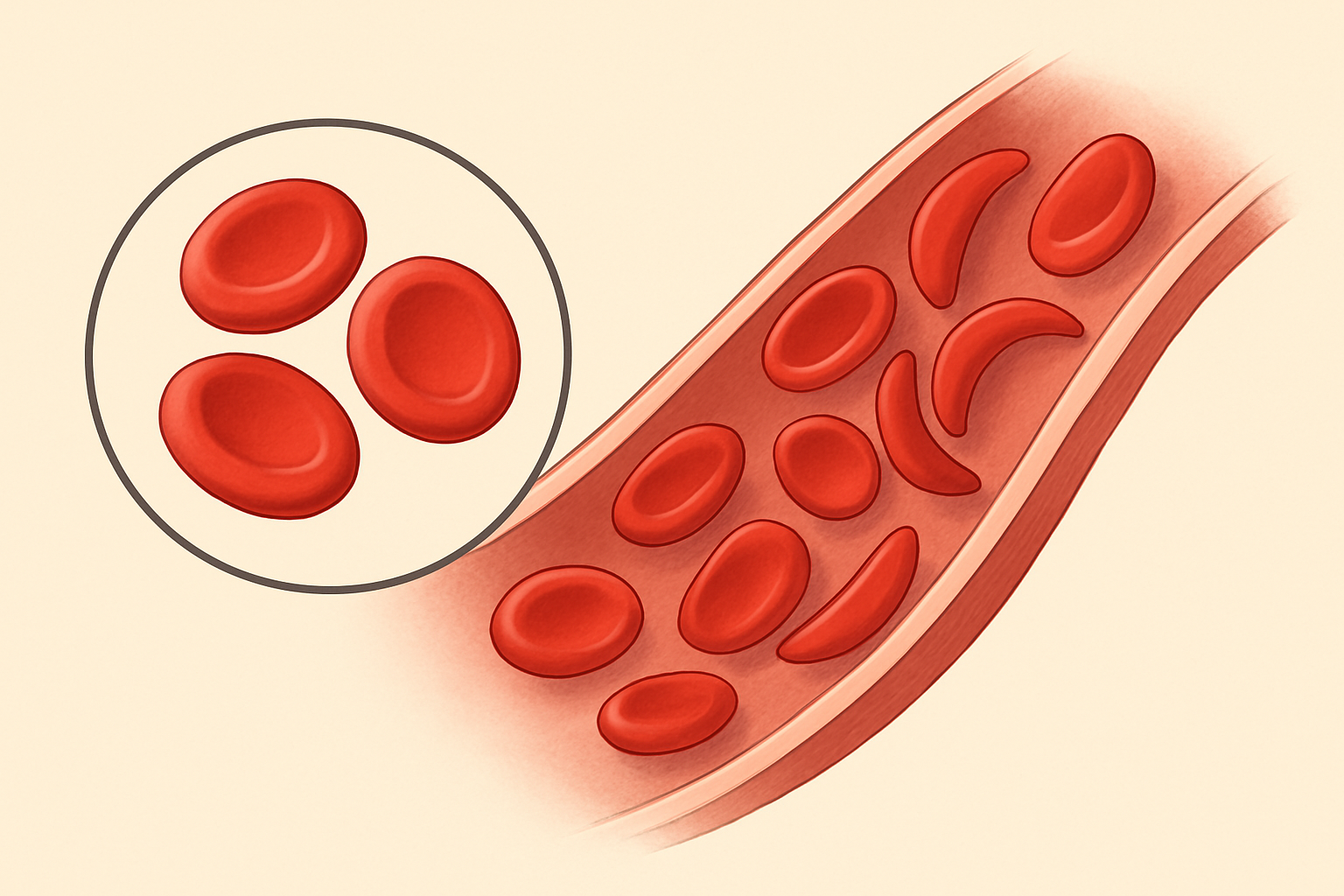
Anemia Mediterranea, more commonly referred to as Thalassemia, is a group of inherited blood disorders resulting in abnormal formation of hemoglobin, the iron-rich protein in red blood cells which carries oxygen to all parts of the body (Khan Academy). These disorders, which are particularly prevalent in the Mediterranean region, can be classified into two main types, alpha and beta Thalassemia, based on the specific globin gene affected (Muncie and Campbell, 2009).
Genetics
Thalassemia is a monogenic disorder, meaning it is caused by defects in a single gene. It is inherited in an autosomal recessive manner, indicating that a child must inherit one defective gene from each parent to develop the disease (ncbi.nlm.nih.gov). The alpha thalassemia results from deletions or mutations in the HBA1 or HBA2 genes, while the beta thalassemia is caused by mutations in the HBB gene (ebi.ac.uk). These mutations lead to reduced or absent synthesis of the corresponding globin chains, disrupting the formation and function of hemoglobin (Weatherall, 2001).
Clinical Manifestations
The clinical manifestations of thalassemia can range from asymptomatic to severe, depending on the number and nature of the mutations (ncbi.nlm.nih.gov). In general, thalassemia causes anemia, which can lead to fatigue, weakness, and pallor. Severe forms can lead to growth retardation, skeletal abnormalities, and increased susceptibility to infections (Muncie and Campbell, 2009). In addition, iron overload, a common complication, can result in damage to the heart, liver, and endocrine system (Weatherall, 2001).
Diagnostic Techniques
Thalassemia is typically diagnosed using a combination of complete blood count (CBC), hemoglobin electrophoresis, and genetic testing. The CBC can reveal microcytic anemia, characterized by reduced mean corpuscular volume and mean corpuscular hemoglobin (Muncie and Campbell, 2009). Hemoglobin electrophoresis can identify abnormal hemoglobin variants, while genetic testing can confirm the specific mutations (khanacademy.org).
Management and Treatment
Management of thalassemia primarily involves regular blood transfusions, iron chelation therapy to remove excess iron, and management of complications (Weatherall, 2001). Hematopoietic stem cell transplantation is currently the only curative treatment, but it carries significant risks and is not available to all patients due to the need for a compatible donor (ncbi.nlm.nih.gov). Gene therapy, which aims to introduce a functional copy of the affected gene into the patient’s cells, holds great promise for the future (ebi.ac.uk).
Conclusion
Thalassemia is a complex genetic disorder with a wide range of clinical manifestations. Although significant advances have been made in its management, it remains a major health burden in many parts of the world. Continued research into novel diagnostic and treatment strategies is crucial to improve the quality of life and prognosis for individuals with this condition.
References
- Muncie, H. L., & Campbell, J. (2009). Alpha and beta thalassemia. American Family Physician, 80(4), 339-344.
- Weatherall, D. J. (2001). The thalassaemias. BMJ: British Medical Journal, 322(7291), 819.
- Khan Academy. Thalassemia. Accessed April 5, 2022.
- National Center for Biotechnology Information. Thalassemia. Accessed April 5, 2022.
- European Bioinformatics Institute. Thalassemia. Accessed April 5, 2022.