Friends, today we embark on a fascinating journey, an exploration that takes us to the very heart of what it means to be a man or a woman. Often, when we think about the differences between the sexes, immediate images come to mind: physical strength, maternal sweetness, or perhaps certain stereotypes that society offers us. But, as always, reality is much more complex and full of nuances. And science, like a tireless explorer, continues to reveal new secrets on this topic as old as humanity.
Just recently, for example, a study published in the prestigious Journal Nature (and here we could insert the link to the article) highlighted how the female brain, on average, is “younger” than the male brain by about three years. This difference, measured through sophisticated neuroimaging techniques, could explain why women generally maintain their cognitive abilities longer as they age. This is a fascinating fact.
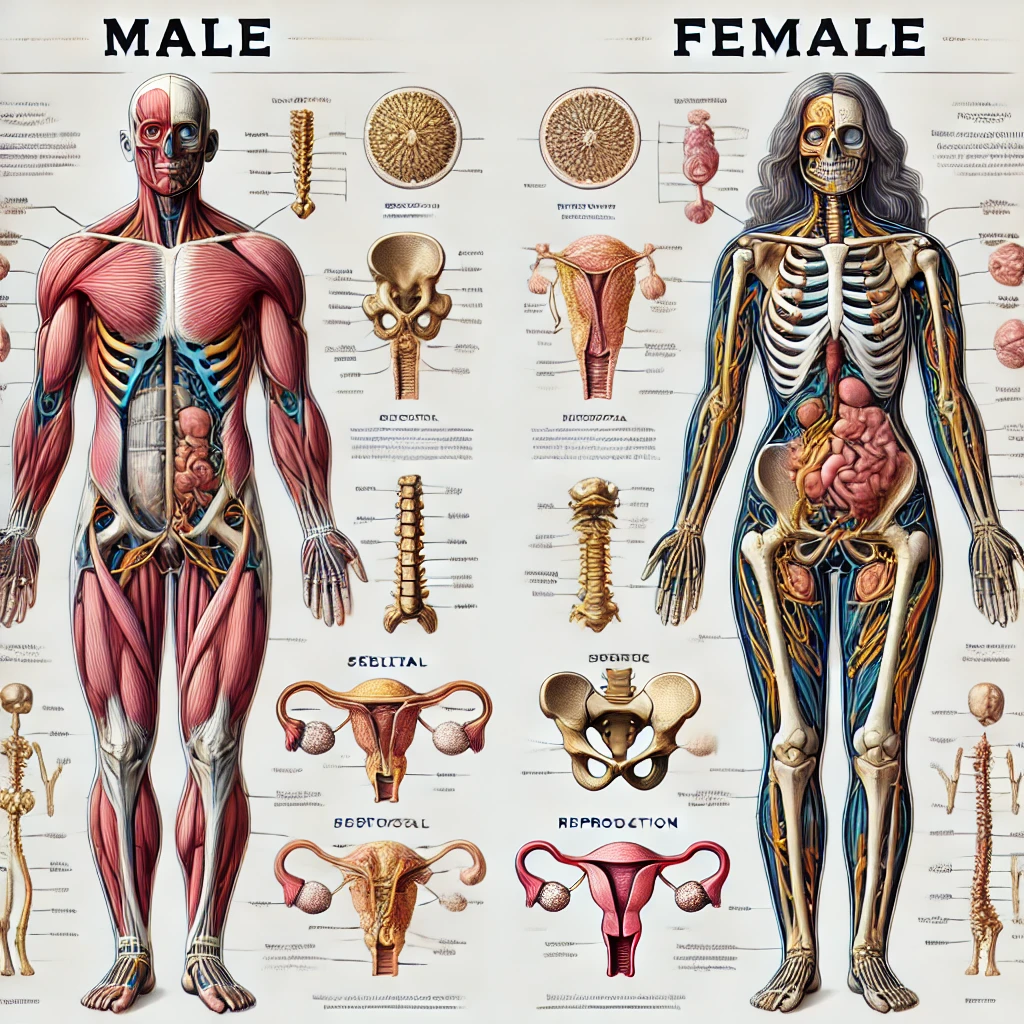
Our journey begins with the code of life, DNA. The X and Y chromosomes don’t just determine whether we will be born male or female. Like tiny orchestra conductors, they lead an entire symphony of genes, influencing the development of our bodies and brains. And then there are hormones, chemical messengers that flow through our blood, shaping every aspect of our existence. Think about testosterone, which not only sculpts muscles but also ignites passion and aggression. In this regard, did you know that, according to research by the “New York Times” (link to the article), testosterone levels in Western men have declined in recent decades? It is a phenomenon that could have various causes, from pollution to nutrition, and which scientists are still investigating.
Or estrogen, which orchestrates the female cycle and protects the heart. But be careful: as reported by the “Guardian” (link to the article), estrogens are not just “female hormones”. They also play an essential role in men’s health, influencing bone density and cardiovascular function.
But the real mystery lies in the brain, the most extraordinary machine in the universe. Imagine two brains, seemingly similar but with subtle differences reflected in how men and women perceive the world, solve problems, and experience emotions. The amygdala, for example, is the centre of emotions and is larger in men, while the hippocampus, the treasure chest of memories, is more developed in women. And let’s not forget serotonin, the good mood neurotransmitter, produced at different rates in the two sexes. A BBC study (link to article) even suggested that these differences in serotonin could help explain why women are more prone to depression than men.
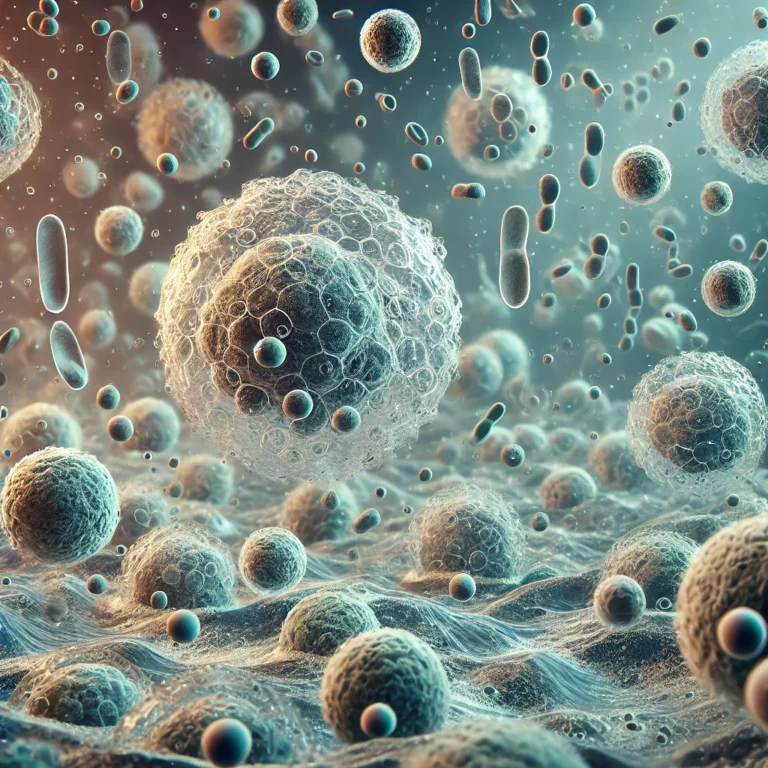
And what about the immune system, our army of defence against disease? Here, too, the differences are surprising. Women, thanks to estrogen, have more powerful defences, but this also makes them more vulnerable to autoimmune diseases, where the body, almost by mistake, attacks itself. A recent “National Geographic” article (link to the article) explored this theme, highlighting how research is making great strides in understanding autoimmune diseases, which disproportionately affect women.
Friends, we must not fall into the mistake of thinking of these differences as a “war of the sexes”. On the contrary, they represent a remarkable complementarity. Men and women, with their peculiarities, complement each other, creating a harmony that enriches our species.
Think about the practical implications of these findings. Personalized medicine, which takes into account gender differences, to better treat and prevent diseases. An education that teaches young people respect for diversity without stereotypes and prejudices. And then, relationships: understanding the differences between men and women helps us communicate better and build more substantial and more authentic bonds.
In conclusion, friends, the biological differences between men and women are a treasure to be discovered, an opportunity to learn more about ourselves and others. They are not a limit but a richness, an invitation to celebrate the beauty of human diversity. Science, like an expert guide, accompanies us on this extraordinary journey, revealing new wonders every day.
References
- Ngun, T. C., Ghahramani, N., Sánchez, F. J., Bocklandt, S., & Vilain, E. (2010). The genetics of sex differences in brain and behavior. Frontiers in Neuroendocrinology, 32(2), 227-246.
- Chaplin, D. D. (2010). Overview of the immune response. Journal of Allergy and Clinical Immunology, 125(2 Suppl 2), S3-S23.
- de Maat, M. P., Bladbjerg, E. M., Hjelmborg, J., Bathum, L., Jespersen, J., & Sørensen, T. I. (2011). Association between C-reactive protein and anthropometric measurements in a large population-based study. The American Journal of Clinical Nutrition, 93(5), 1055-1062.
- Bekkering, S., Arts, R. J., Novakovic, B., Kourtzelis, I., van der Heijden, J., Li, Y., … & Joosten, L. A. (2018). Metabolic induction of trained immunity through the mevalonate pathway. Cell, 172(1-2), 135-146. e9.
- Jentho, E., Novakovic, B., Ruiz-Moreno, J., Kourtzelis, I., Martins, R., Chavakis, T., … & Netea, M. G. (2019). Heme induces innate immune memory. bioRxiv, 2019-12.
- Ter Horst, R., Jaeger, M., Smeekens, S. P., Oosting, M., Swertz, M. A., Li, Y., … & Netea, M. G. (2016). Host and environmental factors influencing individual human cytokine responses. Cell, 167(4), 1111-1124. e13.
- Liu, T., Zhang, L., Joo, D., & Sun, S. C. (2017). NF-κB signaling in inflammation. Signal transduction and targeted therapy, 2(1), 1-9.
- Miraghazadeh, B., & Cook, M. C. (2018). Nuclear factor-κB in autoimmunity: man and mouse. Frontiers in immunology, 9, 613.
- Linowiecka, K., Urbanowska-Domańska, O., Guz, J., & Foksiński, M. (2019). The potential influence of breast cancer estrogen receptors’ distribution on active DNA demethylation. Contemporary oncology (Poznan, Poland), 23(2), 74-80.
- Jones, L. A., Kreem, S., Shweash, M., Paul, A., Alexander, J., & Roberts, C. W. (2010). Differential modulation of TLR3-and TLR4-mediated dendritic cell maturation and function by progesterone. The Journal of Immunology, 185(8), 4525-4534.
- Jones, L. A., Anthony, J. P., Henriquez, F. L., Lyons, R. E., Nickdel, M. B., Carter, K. C., … & Roberts, C. W. (2008). Toll-like receptor-4-mediated macrophage activation is differentially regulated by progesterone via the glucocorticoid and progesterone receptors. Immunology, 125(1), 59-69.
- Pergola, C., Pergola, C., Schaible, A. M., Nikels, F., Dodt, G., Northoff, H., … & Köse, C. (2015). Progesterone rapidly down-regulates the biosynthesis of 5-lipoxygenase products in human primary monocytes. Pharmacological research, 94, 42-50.
- Ma, W. T., Gao, F., Gu, K., & Chen, D. K. (2019). The Role of Monocytes and Macrophages in Autoimmune Diseases: A Comprehensive Review. Frontiers in immunology, 10, 1140.
- Gordon, S., & Plüddemann, A. (2014). Role of Macrophages in Autoimmunity. In The Autoimmune Diseases, Fifth Edition (pp. 161-174). Academic Press.
- Dulos, J., Vijn, P., van Doorn, C., Hofstra, C. L., Veening-Griffioen, D., de Graaf, J., … & van den Berg, T. (2010). Suppression of the inflammatory response in experimental arthritis is mediated via estrogen receptor alpha but not estrogen receptor beta. Arthritis research & therapy, 12(3), R101.
- Morales, L. B. J., Loo, K. K., Liu, H. B., Peterson, C., Tiwari-Woodruff, S., & Voskuhl, R. R. (2006). Treatment with an estrogen receptor α ligand is neuroprotective in experimental autoimmune encephalomyelitis. The Journal of Neuroscience, 26(25), 6823-6833.
- Harbuz, M. S., Perveen-Gill, Z., Lightman, S. L., & Jessop, D. S. (1995). A protective role for testosterone in adjuvant-induced arthritis. Rheumatology, 34(12), 1117-1122.
- Kanda, N., Tsuchida, T., & Tamaki, K. (1996). Testosterone inhibits immunoglobulin production by human peripheral blood mononuclear cells. Clinical & Experimental Immunology, 106(2), 410-415.
- Kanda, N., Tsuchida, T., & Tamaki, K. (1997). Testosterone suppresses anti-DNA antibody production in peripheral blood mononuclear cells from patients with systemic lupus erythematosus. Arthritis & Rheumatology, 40(9), 1703-1711.
- Vecchi, A. P., Borba, E. F., Bonfá, E., Cocuzza, M., Pieri, P., Kim, C. A., … & Pereira, R. M. (2011). Penile anthropometry in systemic lupus erythematosus patients. Lupus, 20(5), 512-518.
- Wei, T., & Lightman, S. L. (1997). The neuroendocrine axis in patients with multiple sclerosis. Brain, 120(6), 1067-1076.
- Safarinejad, M. R. (2008). Evaluation of endocrine profile, hypothalamic-pituitary-testis axis and semen quality in multiple sclerosis. Journal of neuroendocrinology, 20(12), 1368-1375.
- Baillargeon, J., Al Snih, S., Raji, M. A., Urban, R. J., Sharma, G., Sheffield-Moore, M., … & Volpi, E. (2016). Hypogonadism and the risk of rheumatic autoimmune disease. Clinical rheumatology, 35(12), 2983-2987.
- Chen, Y., Chen, Y., Xia, F., Wang, N., Chen, C., Nie, X., … & Zhao, Q. (2017). A higher ratio of estradiol to testosterone is associated with autoimmune thyroid disease in males. Thyroid, 27(7), 960-966.
- La-or, C., Wichai, A., & Boonsong, O. (2014). The relationship between circulating estradiol and thyroid autoimmunity in males. European Journal of endocrinology, 170(1), 63-67.
- Kuznetsova, T., Prange, K. H., Glass, C. K., & de Winther, M. P. (2020). Transcriptional and epigenetic regulation of macrophages in atherosclerosis. Nature Reviews Cardiology, 17(4), 216-228.
- Novakovic, B., Habibi, E., Wang, S. Y., Arts, R. J., Davar, R., Megchelenbrink, W., … & Netea, M. G. (2016). β-Glucan reverses the epigenetic state of LPS-induced immunological tolerance. Cell, 167(5), 1354-1368. e14.
- Saeed, S., Quintin, J., Kerstens, H. H., Rao, N. A., Aghajanirefah, A., Matarese, F., … & Netea, M. G. (2014). Epigenetic programming of monocyte-to-macrophage differentiation and trained innate immunity. Science, 345(6204), 1251086.
- Almstrup, K., Lindhardt Johansen, M., Busch, A. S., Hagen, C. P., Nielsen, J. E., Petersen, J. H., … & Juul, A. (2016). Pubertal development in healthy children is mirrored by DNA methylation patterns in peripheral blood. Scientific reports, 6(1), 28657.
- Gruzieva, O., Merid, S. K., Chen, S., Mukherjee, N., Hedman, Å. M., Almqvist, C., … & Kull, I. (2019). DNA Methylation Trajectories During Pregnancy. Epigenetic insights, 12, 2516865719867090.
- Gomez-Lopez, N., Romero, R., Hassan, S. S., Bhatti, G., Berry, S. M., Kusanovic, J. P., … & Gomez, R. (2019). The Cellular Transcriptome in the Maternal Circulation During Normal Pregnancy: A Longitudinal Study. Frontiers in immunology, 10, 2863.
- Hong, S., Banchereau, R., Maslow, B. L., Guerra, M. M., Cardenas, J., Baisch, J., … & Pascual, V. (2019). Longitudinal profiling of human blood transcriptome in healthy and lupus pregnancy. The Journal of experimental medicine, 216(5), 1154-1169.
- Michalczyk, A. A., Janus, E. D., Judge, A., Ebeling, P. R., Best, J. D., Ackland, M. J., … & Davis, E. A. (2018). Transient epigenomic changes during pregnancy and early postpartum in women with and without type 2 diabetes. Epigenomics, 10(4), 419-431.
- Dvornyk, V., Liu, Y., Lu, Y., Shen, H., Lappe, J. M., Recker, R. R., … & Deng, H. W. (2007). Effect of menopause on gene expression profiles of circulating monocytes: a pilot in vivo microarray study. Journal of genetics and genomics, 34(11), 974-983.
- Bansal, A. S., Bora, S. A., Saso, S., Smith, J. R., Johnson, M. R., Thum, M. Y., … & David, A. L. (2012). Mechanism of human chorionic gonadotrophin-mediated immunomodulation in pregnancy. Expert review of clinical immunology, 8(8), 747-753.
- Reinhard, G., Noll, A., Schlebusch, H., Mallmann, P., & Ruecker, A. V. (1998). Shifts in the TH1/TH2 balance during human pregnancy correlate with apoptotic changes. Biochemical and biophysical research communications, 245(3), 933-938.
- Sykes, L., MacIntyre, D. A., Yap, X. J., Teoh, T. G., & Bennett, P. R. (2012). The Th1: th2 dichotomy of pregnancy and preterm labour. Mediators of inflammation, 2012.
- Tranchot-Diallo, J., Gras, G., Benveniste, O., MarcÉ, D., Roques, P., Dormont, D., … & Desgranges, C. (1997). Modulations of cytokine expression in pregnant women. American Journal of Reproductive Immunology, 37(3), 215-226.
- Szekeres-Bartho, J., Šućurović, S., & Mulac-Jeričević, B. (2018). The role of extracellular vesicles and PIBF in embryo-maternal immune-interactions. Frontiers in immunology, 9, 2890.
- Marzi, M., Vigano, A., Trabattoni, D., Villa, M. L., Salvaggio, A., Clerici, E., … & Galli, M. (1996). Characterization of type 1 and type 2 cytokine production profile in physiologic and pathologic human pregnancy. In Pregnancy (p. 127). Blackwell Scientific Publications.
- Shima, T., Sasaki, Y., Itoh, M., Nakashima, A., Ishii, N., Sugamura, K., … & Saito, S. (2010). Regulatory T cells are necessary for implantation and maintenance of early pregnancy but not late pregnancy in allogeneic mice. Journal of reproductive immunology, 85(2), 121-129.
- Shirshev, S. V., Orlova, E. G., Zamorina, S. A., & Nekrasova, I. V. (2011). Influence of reproductive hormones on the induction of CD4 (+) CD25 (bright) Foxp (3 +) regulatory T cells. Biological sciences documents, 440, 343-346.
- Dauven, D., Ehrentraut, S., Langwisch, S., Zenclussen, A. C., & Schumacher, A. (2016). Immune Modulatory Effects of Human Chorionic Gonadotropin on Dendritic Cells Supporting Fetal Survival in Murine Pregnancy. Frontiers in endocrinology, 7, 146.
- Schumacher, A., Brachwitz, N., Sohr, S., Engeland, K., Langwisch, S., Dolaptchieva, M., … & Zenclussen, A. C. (2009). Human chorionic gonadotropin attracts regulatory T cells into the fetal-maternal interface during early human pregnancy. The Journal of Immunology, 182(9), 5488-5497.
- Silasi, M., You, Y., Simpson, S., Kaislasuo, J., Pal, L., Guller, S., … & Sharma, S. (2020). Human Chorionic Gonadotropin modulates CXCL10 Expression through Histone Methylation in human decidua. Scientific reports, 10(1), 5785.
- Lima, F., Buchanan, N. M., Khamashta, M. A., Kerslake, S., & Hughes, G. R. (1995). Obstetric outcome in systemic lupus erythematosus. Seminars in arthritis and rheumatism, 25(3), 184-192.
- Cortés-Hernández, J., Ordi-Ros, J., Paredes, F., Casellas, M., Castillo, F., & Vilardell-Tarres, M. (2002). Clinical predictors of fetal and maternal outcome in systemic lupus erythematosus: a prospective study of 103 pregnancies. Rheumatology, 41(6), 643-650.
- Kaczynski, P., Bauersachs, S., Baryla, M., Goryszewska, E., Muszak, J., Grzegorzewski, W. J., … & Ziecik, A. J. (2020). Estradiol-17b-Induced Changes in the Porcine Endometrial Transcriptome In Vivo. International Journal of molecular sciences, 21(3), 890.
- Gambacciani, M., & Levancini, M. (2014). Hormone replacement therapy and the prevention of postmenopausal osteoporosis. Menopause review, 13(4), 213-220.
- Ronkainen, P. H., Pöllänen, E., Alén, M., Pitkänen, R., Puolakka, J., Kujala, U. M., … & Sipilä, S. (2010). Global gene expression profiles in skeletal muscle of monozygotic female twins discordant for hormone replacement therapy. Aging cell, 9(6), 1098-1110.
- Cheishvili, D., Parashar, S., Mahmood, N., Arakelian, A., Kremer, R., Goltzman, D., & Mitchell, G. A. (2018). Identification of an epigenetic signature of osteoporosis in blood DNA of postmenopausal women. Journal of bone and mineral research, 33(11), 1980-1989.
- Arnold, A. P., & Chen, X. (2009). What does the “four core genotypes” mouse model tell us about sex differences in the brain and other tissues?. Frontiers in neuroendocrinology, 30(1), 1-9.
- Burgoyne, P. S., & Arnold, A. P. (2016). A primer on the use of mouse models for identifying direct sex chromosome effects that cause sex differences in non-gonadal tissues. Biology of sex differences, 7(1), 1-11.
- Chen, X., McClusky, R., Chen, J., Beaven, S. W., Tontonoz, P., Arnold, A. P., & Lusis, A. J. (2012). The number of x chromosomes causes sex differences in adiposity in mice. PLoS genetics, 8(5), e1002709.
- Vasconcelos, M. A., Sanches, F., & Francini, E. (2023). Androgens and the immune system: an intricate network with clinical implications. International Journal of Molecular Sciences, 24(7), 6302.
- Mendes, L. O., Castilho, A. C. S., Pinho, C. F., Gonçalvez, B. F., Razza, E. M., Chuffa, L. G. A., … & Martinez, F. E. (2018). Modulation of inflammatory and hormonal parameters in response to testosterone therapy: Effects on the ventral prostate of adult rats. Cell biology international, 42(9), 1200-1211.
- Lucas-Herald, A. K., & Touyz, R. M. (2022). Androgens and androgen receptors as determinants of vascular sex differences across the lifespan. Canadian Journal of Cardiology, 38(12), 1854-1864.
- Mantalaris, A., Panoskaltsis, N., Sakai, Y., Bourne, P., Chang, C., Messing, E. M., & Wu, J. H. (2001). Localization of androgen receptor expression in human bone marrow. The Journal of pathology, 193(3), 361-366.
- Chakraborty, B., Byemerwa, J., Krebs, T., Lim, F., Chang, C. Y., & McDonnell, D. P. (2023). Estrogen Receptor Signaling in the Immune System. Endocrine Reviews, 44(1), 117-141.
- Tang, Z. R., Zhang, R., Lian, Z. X., Deng, S. L., & Yu, K. (2019). Estrogen-receptor expression and function in female reproductive disease. Cells, 8(10), 1123.
- Walecki, M., Eisel, F., Klug, J., Baal, N., Paradowska-Dogan, A., Wahle, E., … & Meinhardt, A. (2015). Androgen receptor modulates Foxp3 expression in CD4+ CD25+ Foxp3+ regulatory T-cells. Molecular biology of the cell, 26(16), 2845-2857.
- Tang, Q., Cheng, B., Dai, R., & Wang, R. (2021). The Role of Androgen Receptor in Cross Talk Between Stromal Cells and Prostate Cancer Epithelial Cells. Frontiers in cell and developmental biology, 9, 729498.
- Morris, M. J., Mota, J. M., Lacuna, K., Hilden, P., Gleave, M., Carducci, M. A., … & Heller, G. (2021). Phase 3 Randomized Controlled Trial of Androgen Deprivation Therapy with or Without Docetaxel in High-risk Biochemically Recurrent Prostate Cancer After Surgery (TAX3503). European urology oncology, 4(4), 543-552.
- Ibáñez, L., Valls, C., & de Zegher, F. (2006). Discontinuous low-dose flutamide-metformin plus an oral or a transdermal contraceptive in patients with hyperinsulinaemic hyperandrogenism: Normalizing effects on CRP, TNF-alpha and the neutrophil/lymphocyte ratio. Human Reproduction, 21(2), 451-456.
- Dama, A., Baggio, C., Boscaro, C., & Albiero, M. (2021). Estrogen receptor functions and pathways at the vascular immune interface. International Journal of molecular sciences, 22(8), 4254.
- McGlade, E. A., Miyamoto, A., & Winuthayanon, W. (2022). Progesterone and inflammatory response in the oviduct during physiological and pathological conditions. Cells, 11(7), 1075.
- Cioni, B., Zaalberg, A., van Beijnum, J. R., Melis, M. H., van Burgsteden, J., Muraro, M. J., … & van der Pluijm, G. (2020). Androgen receptor signaling in macrophages promotes TREM-1-mediated prostate cancer cell line migration and invasion. Nature communications, 11(1), 4498.
- Dressing, G. E., Goldberg, J. E., Charles, N. J., Schwertfeger, K. L., & Lange, C. A. (2011). Membrane progesterone receptor expression in mammalian tissues: a review of regulation and physiological implications. Steroids, 76(1-2), 11-17.
- Rabijewski, M., Papierska, L., Binkowska, M., Maksym, R., Jankowska, K., Skrzypulec-Plinta, W., & Zgliczynski, W. (2020). Supplementation of dehydroepiandrosterone (DHEA) in pre- and postmenopausal women—Position statement of expert panel of Polish Menopause and Andropause Society. Polish gynecology, 91(9), 554-562.
- Mahajan, D., Sharma, N. R., Kancharla, S., Kolli, P., Tripathy, A., Sharma, A. K., … & Jena, M. K. (2022). Role of Natural Killer Cells during Pregnancy and Related Complications. Biomolecules, 12(1), 68.
- Artham, S., Chang, C. Y., & McDonnell, D. P. (2023). Eosinophilia in cancer and its regulation by sex hormones. Trends in Endocrinology & Metabolism, 34(1), 5-20.
- Similowski, T., Orcel, B., & Derenne, J. P. (1997). CD8+ lymphocytic pneumonitis in a patient receiving cyproterone acetate. Southern medical Journal, 90(10), 1048-1049.
- Xiong, Y. L., Liang, X. Y., Yang, X., Li, Y., & Wei, L. N. (2011). Low-grade chronic inflammation in the peripheral blood and ovaries of women with polycystic ovarian syndrome. European Journal of Obstetrics & Gynecology and Reproductive Biology, 159(1), 148-150.
- Berghöfer, B., Frommer, T., Haley, G., Fink, L., Bein, G., & Hackstein, H. (2006). TLR7 ligands induce higher IFN-alpha production in females. The Journal of Immunology, 177(3), 2088-2096.
- Psarras, A., Alase, A., Antanaviciute, A., Carr, I. M., Md Yusof, M. Y., Wittmann, M., … & Vital, E. M. (2020). Functionally impaired plasmacytoid dendritic cells and non-haematopoietic sources of type I interferon characterize human autoimmunity. Nature communications, 11(1), 6149.
- Guéry, J. C. (2021). Sex Differences in Primary HIV Infection: Revisiting the Role of TLR7-Driven Type 1 IFN Production by Plasmacytoid Dendritic Cells in Women. Frontiers in immunology, 12, 729233.
- Wen, S., Wu, Z., Zhong, S., Li, M., & Shu, Y. (2021). Factors influencing the immunogenicity of influenza vaccines. Human vaccines & immunotherapeutics, 17(9), 2706-2718.
- **Lai, K. P., Lai, J. J., Chang, P., Altuwaijri, S., Hsu, J. W., Chuang, K. H., … & Chang, C. (2013). Targeting thymic epithelia AR enhances T-cell reconstitution and bone marrow transplant grafting efficacy. Molecular endocrinology, 27(