Introduction
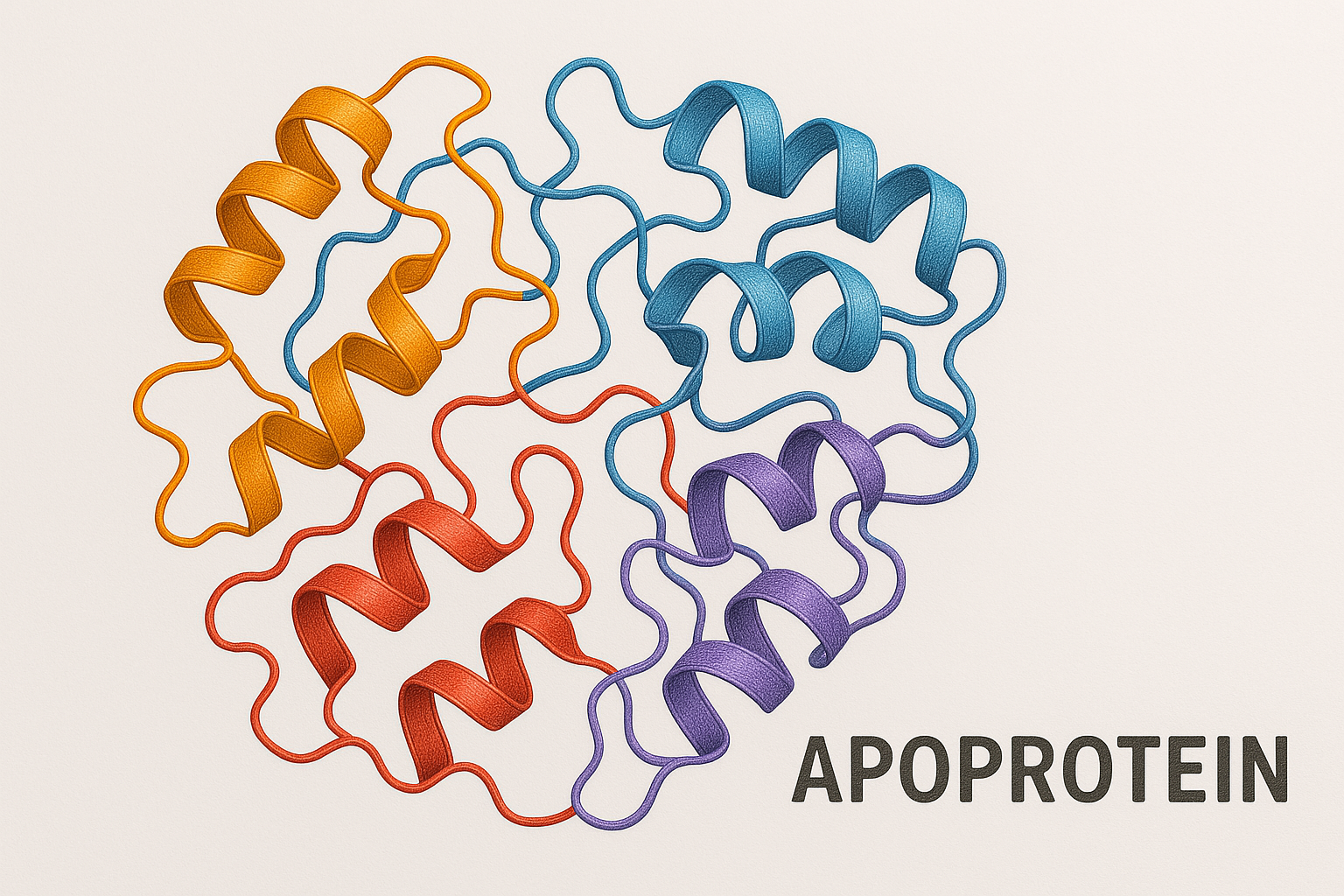
Apoproteins are lipids, which are insoluble in water, rely on these protein-bound forms for circulation in the aqueous environment of our bodies. Apoproteins play a pivotal role in lipid transport, metabolism, and homeostasis, and therefore have significant implications for human health and disease, particularly cardiovascular disease.
The Structure and Function of Apoproteins
Apoproteins are primarily synthesized in the liver and the intestine, and they bind to lipids to form lipoprotein particles (Mahan & Escott-Stump, 2008). Each lipoprotein particle consists of a core of neutral lipids, primarily triglycerides and cholesterol esters, surrounded by a monolayer of phospholipids, free cholesterol, and apoproteins (Dashty, 2013).
Apoproteins serve several crucial functions. First, they provide structural stability to the lipoprotein particle, allowing it to remain intact during circulation. Second, apoproteins serve as ligands for cell surface receptors, facilitating the uptake of lipids by cells. Lastly, they act as cofactors for enzymes involved in lipid metabolism (Dashty, 2013).
Classes of Apoproteins
Apoproteins are classified into various types, including ApoA, ApoB, ApoC, and ApoE, each of which is associated with specific types of lipoproteins and functions.
- **ApoA**: This class, including ApoA-I and ApoA-II, is primarily associated with high-density lipoprotein (HDL). ApoA-I is crucial in the process of reverse cholesterol transport, where it helps to remove excess cholesterol from tissues and deliver it to the liver for excretion (Zannis et al., 2006).
- **ApoB**: This includes ApoB-48, found in chylomicrons, and ApoB-100, found in very low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), and low-density lipoprotein (LDL). ApoB-100 is essential for the uptake of LDL by the liver and other tissues (Segrest et al., 2000).
- **ApoC**: This class includes ApoC-II and ApoC-III. ApoC-II is a necessary cofactor for lipoprotein lipase, which hydrolyzes triglycerides in lipoproteins, while ApoC-III inhibits this process (Ooi et al., 2015).
- **ApoE**: ApoE mediates the clearance of chylomicron remnants and VLDL from the circulation and is also involved in the transport of lipids to the brain (Mahley, 2016).
Apoproteins and Disease
Given their central role in lipid metabolism, mutations and dysregulation in apoproteins are often associated with lipid disorders and cardiovascular disease. For example, elevated levels of ApoB, which is present in all atherogenic (plaque-forming) lipoproteins, are a strong predictor of coronary heart disease (Sniderman et al., 2001). On the other hand, ApoA-I, associated with HDL’s protective effects against heart disease, is often found to be lower in individuals with cardiovascular disease (Barter et al., 2004).
Conclusion
Apoproteins play a fundamental role in lipid transport and metabolism. Understanding their structure, function, and the implications of their dysregulation offers valuable insights into the pathophysiology of metabolic and cardiovascular diseases. Therefore, apoproteins serve not only as diagnostic markers but also as potential therapeutic targets in these conditions.
Test Your Knowledge on Apoproteins!
Answer the following questions to check your understanding of the article on apoproteins and lipid transport.
References
- Barter, P., Gotto, A. M., LaRosa, J. C., Maroni, J., Szarek, M., Grundy, S. M., … & Fruchart, J. C. (2004). HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. New England Journal of Medicine, 351(13), 1293-1303.
- Dashty, M. (2013). A quick look at biochemistry: lipoprotein metabolism. Clinical Biochemistry, 46(15), 1339-1352.
- Mahan, L.K., Escott-Stump, S. (2008). Krause’s Food & Nutrition Therapy. St. Louis, MO: Elsevier.
- Mahley, R. W. (2016). Apolipoprotein E: from cardiovascular disease to neurodegenerative disorders. Journal of Molecular Medicine, 94(7), 739-746.
- Ooi, E. M., Barrett, P. H., Chan, D. C., & Watts, G. F. (2015). Apolipoprotein C-III: understanding an emerging cardiovascular risk factor. Clinical Science, 114(10), 661-671.
- Segrest, J. P., Jones, M. K., De Loof, H., Brouillette, C. G., Venkatachalapathi, Y. V., & Anantharamaiah, G. M. (2000). The amphipathic helix in the exchangeable apolipoproteins: a review of secondary structure and function. Journal of Lipid Research, 33(2), 141-166.
- Sniderman, A. D., Pedersen, T., & Kjekshus, J. (2001). Putting low-density lipoproteins at center stage in atherogenesis. The American Journal of Cardiology, 88(7), 5-9.
- Zannis, V. I., Chroni, A., & Krieger, M. (2006). Role of apoA-I, ABCA1, LCAT, and SR-BI in the biogenesis of HDL. Journal of Molecular Medicine, 84(4), 276-294.